To learn more about OCD therapy, you can schedule a free, no obligation, phone consultation with Dr. Isabelle Bauer.

Have you ever experienced an unwanted, intrusive thought or doubt?
“what if I punch the stranger next to me?“
“what if I impulsively and inappropriately touch someone?”
“am I real? Do I really exist? What if this is all a dream?”
“what if I jump off the balcony?”
“what if I didn’t turn off the stove or lock the door?”
“what if I made an irreversible mistake?”
“what if I wrote something inappropriate or offensive in the email?”
Have any unwanted, intrusive images ever popped into your head?
The image of being in a car crash
The image of pushing someone onto subway tracks
The image of stabbing your partner
The image of blurting out a slur or saying something offensive

If you answered yes to any of these, then you’re like the rest of us. The human brain generates thousands of thoughts & images every moment of every day. Some are intentional or automatic, while others are experienced as unwanted & intrusive. The thoughts that pop into our minds at any given time range from positive, to neutral, to negative. This is a natural part of being a human & having a brain – it will offer us the full spectrum of thoughts, ranging from mundane, interesting, exciting, rational, all the way to irrational, weird, inappropriate, & even obscene, disturbing, & shocking.
How a person responds to an intrusive thought or image can make the difference between whether they move on with their day or move on to develop OCD.
Most people will experience intrusive thoughts on occasion. Most of the time, these thoughts go largely unnoticed, they may be quickly dismissed, or they may trigger a brief pang of emotion before the mind moves on to the next thought or preoccupation. For others, intrusive thoughts can literally stop them in their tracks, and they may start to wonder… “how could I have such an awful thought?”, “what does this mean about me?”, or “what if I want to act on this thought?”. How a person responds to an intrusive thought or image can make the difference between whether they move on with their day or move on to develop OCD.
WHAT IS OCD?
Obsessive-compulsive disorder is a common mental health challenge – approximately 1 in 40 adults is affected by OCD in their lifetime. Women are more likely than men to develop OCD, with higher risk during pregnancy & postpartum. While the onset of OCD usually starts gradually during childhood, it typically develops in adolescence and early adulthood.
1 in 40 adults is affected by OCD in their lifetime.
It is not enough to experience intrusive thoughts or to engage in repetitive behaviors sometimes to be diagnosed with OCD. Similarly, a preference for cleanliness, orderliness, or perfectionism is not OCD, despite the common phrase “I’m so OCD” that people often use to refer to such tendencies. Unfortunately, this reference trivializes the disorder & minimizes the associated distress and impairment.
Obsessive-Compulsive Disorder involves the presence of recurrent intrusive & unwanted thoughts, urges, or images that cause significant distress and anxiety. These intrusive thoughts are ego-dystonic, which means that they are unwanted & distressing thoughts or images that go against people’s core values and beliefs. Given the distress or anxiety these thoughts can trigger, people attempt to suppress or neutralize those thoughts with the use of compulsions. Compulsions involve repetitive behaviors that a person feels driven to perform to get rid of the obsession, reduce the anxiety, or prevent some negative event or consequences. These compulsions are often performed in a rigid or ritualistic manner. The intrusive thoughts & compulsions are time-consuming, taking up more than one hour per day, & lead to significant distress or impairment in functioning.
OCD can take on many forms, such that the content of intrusive thoughts & the nature of compulsions can vary across individuals. The content of intrusive thoughts can also change over time, depending on a person’s unique circumstances, the stressors they face, or their stage of life. It is also important to note that OCD targets what is most important to individuals. For example, for individuals who value being a kind & caring person, unwanted thoughts about harming others may be especially distressing. For people who have a deep attachment to loved ones, the thought of illness & death may be especially difficult to bear. For others who value their faith/religion, an intrusive blasphemous thought or image may feel deeply unsettling. While intrusive thoughts & compulsions can be boundless in their content, variety, and specific manifestation, it can be helpful to categorize them into some common themes.
TYPES OF OBSESSIONS:
Contamination Obsessions – unwanted thoughts of contracting or spreading disease through physical contamination by germs/viruses, bodily fluids (saliva, blood, urine, feces) or environmental/chemical contamination (toxins such as household cleaners, pesticides, asbestos, mold). This can also include the fear of getting “dirty” through contact with substances (e.g. glue, grease, dirt, garbage).
Violent (Harm) Obsessions – unwanted thoughts of harming oneself, loved ones, or strangers (e.g. stabbing, choking).
Sexual Obsessions – unwanted thoughts about engaging in inappropriate and illegal sexual acts. This can include pedophilia, incest, and sexual aggression.
Religious/Moral Scrupulosity Obsessions – unwanted thoughts related to sin, blasphemy, or behaving in an immoral way that violates moral and ethical codes and standards.
Identity Obsessions – intrusive thoughts and doubts about one’s sexual orientation, gender identity, authentic identity, or moral character.
Perfectionism or “Just Right” Obsessions – refers to the strong need for order, precision, symmetry, or completeness. This can involve a physical or mental feeling (e.g. needing to address an internal feeling of being “off” or “not quite right”).
Existential Obsessions – unwanted thoughts related to big existential questions such as the meaning of life, the nature of reality, or ruminating on death and the afterlife.
Relationship Obsessions – intrusive doubts about one’s relationship, such as doubting whether someone is with the right partner, whether their love is sufficient to remain in the relationship, whether they are compatible enough, whether there is someone else out there for them.
Sensorimotor/Somatic OCD – involves a hyper-focus on automatic and involuntary body functions or sensations, such as swallowing, blinking, breathing, or heartbeat. This can include a hyper-focus on natural bodily sensations such as eye floaters or skin sensations.
Responsibility Obsessions – intrusive thoughts about being responsible for harm, mistakes, accidents, or moral/social offences.
COMMON COMPULSIONS:
Washing & Cleaning – repeatedly & excessively washing or cleaning if someone thinks they came into contact with a contaminant (e.g. bodily fluid, blood, chemicals, dirt, germs/viruses). This can involve hand washing, showering, cleaning things/surfaces.
Checking – repeatedly & excessively checking doors, locks, appliances to make sure they are turned off. It can involve checking emails, messages, work or personal documents to ensure there are no mistakes, typos, or that they didn’t inadvertently write something offensive or inappropriate.
Mental Compulsions (mental review) – repeatedly and excessively replaying conversations, memories, sequences of past events, past behaviors to ensure nothing untoward happened to oneself or others.
Repeating & Counting – Counting, praying, repeating specific words/sentences/mantras/behaviors. This can be done according to certain rules or rituals such as counting to a certain number, repeating something a specific number of times, etc.
Symmetry, Ordering & Arranging – arranging or organizing items according to specific rules (e.g. by colour, size), ensuring that objects are placed in a symmetrical manner, or ordering things. This can be done to achieve a “just right” feeling or to ensure perfection.
Reassurance Seeking (from self or others) – asking people for reassurance that they are safe, that they did not make a mistake or cause harm/offence, and that “everything is ok”. It can include online researching & using ChatGPT. Self-reassurance can include mentally reviewing actions/memories/conversations.
Neutralizing or Suppressing Thoughts – Countering a “bad” thought by replacing it with a positive/neutral thought or deliberately pushing away a “bad” thought.
Avoidance – excessive avoidance of places, people, sensations, or situations that can trigger intrusive thoughts & anxiety (e.g. avoiding using knives for fear of harming someone, avoiding public places to avoid contamination by germs/viruses/dirt).
GETTING STUCK IN THE OCD LOOP
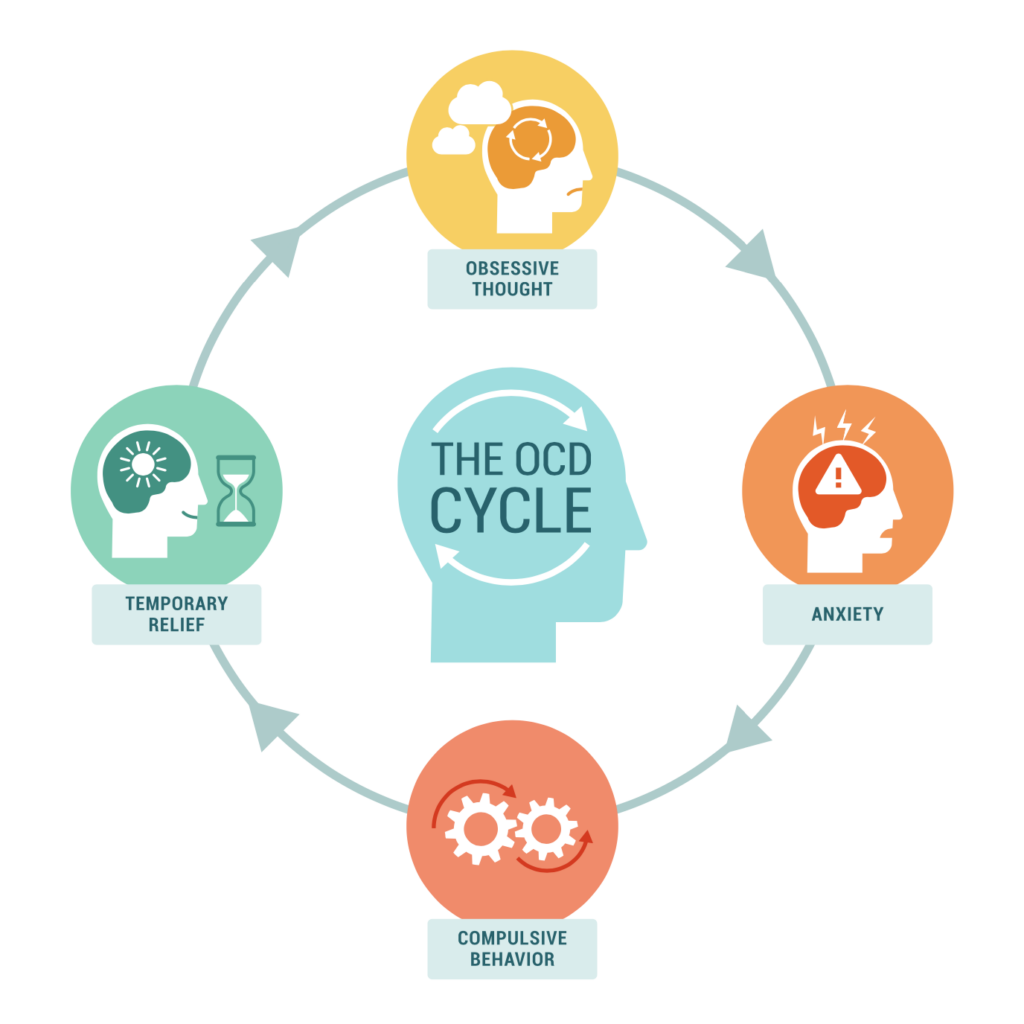
While many people will see intrusive thoughts for what they are – random, insignificant noise produced by our minds – others get caught up in the OCD loop.
What you resist, persists.
They experience an intrusive thought that triggers significant anxiety and distress. This leads them to perform a compulsion to suppress or neutralize the thought. They learn that engaging in the compulsion temporarily relieves anxiety or distress, which reinforces this behavior as a coping strategy in the future. The next time they experience an intrusive thought, it will trigger just as much if not more anxiety and individuals will revert back to using compulsive behaviors to manage the distress associated with the obsession. Each time they engage in the compulsion, this reinforces and perpetuates the OCD loop, making it increasingly difficult to break out of it over time. In essence, “what you resist, persists”.
OCD TREATMENTS
While OCD can be very distressing and debilitating, there are several psychological and pharmacological treatments that can be effective. Research shows that the gold standard psychological treatment for OCD involves Exposure & Response Prevention (ERP) while the gold standard pharmacological treatment involves the use of SSRIs. Generally, ERP is considered more effective than medication alone for treating OCD. This is especially true in the long term, as ERP teaches skills that individuals can continue to practice post-treatment to build on their treatment gains, whereas there is a higher risk of symptom relapse upon medication discontinuation. While ERP is highly effective, for more severe cases of OCD, a combination of ERP and medication may be recommended for the best outcomes.
Exposure & Response Prevention (ERP) is a form of CBT therapy that involves gradually confronting triggers (thoughts, images, or situations) that provoke anxiety or distress (exposure), while deliberately refraining from performing the compulsions (response prevention). If fighting the mind by suppressing thoughts, avoiding triggers, & engaging in compulsions fuels OCD, then it stands to reason that leaning into uncomfortable thoughts & emotions through exposure can disrupt the OCD loop & take the power out of intrusive thoughts. This is supported by research which shows that with repeated ERP practices, individuals can learn to break the OCD loop by learning that anxiety will reduce on its own without the need for compulsions.
Leaning into uncomfortable thoughts & emotions through exposure can disrupt the OCD loop & take the power out of intrusive thoughts.
For those who continue to struggle with significant OCD symptoms despite ERP treatment or for those whose symptoms are so severe that it makes it difficult to fully engage with ERP treatment, there are alternative approaches that can also be helpful, including Acceptance & Commitment Therapy (ACT) or Inference-Based Cognitive Behavioral Therapy (I-CBT).